485
Views & Citations10
Likes & Shares
Objective: The purpose of this study was to introduce the placement of a ramal plate in the retromolar fossa as a novel temporary skeletal anchorage device (TSAD) for correction of skeletal Class III malocclusion by distalization of mandibular dentition among Yemeni patients of Sana`a university.
Conclusion: The mandibular molar showed a significant amount of distalization. A ramal plate may be a viable device for mandibular total arch distalization in Class III patients who are reluctant to undergo orthognathic surgery.
Keywords: Distalization, Mandibular dentition, Ramal plate, Skeletal class III malocclusion, Yemen
Abbreviations: CBCT: Cone Beam CT Scan Tomography; ICC: Intraclass Correlation Coefficient; M: Mean; Max: Maximum; Min: Minimum; SD: Standard Deviation; TSAD: Temporary Skeletal Anchorage Device; X2: Chi Square
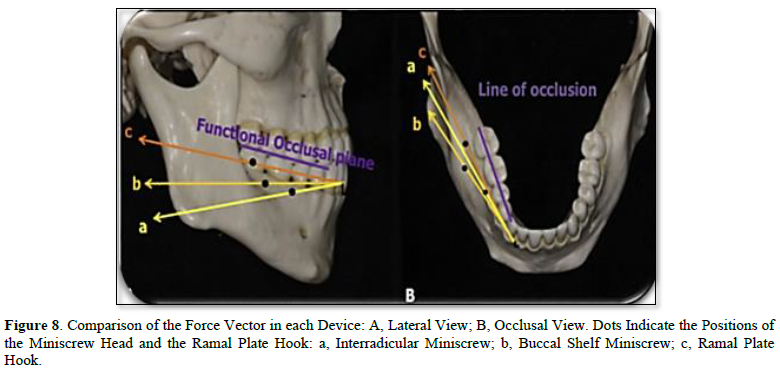
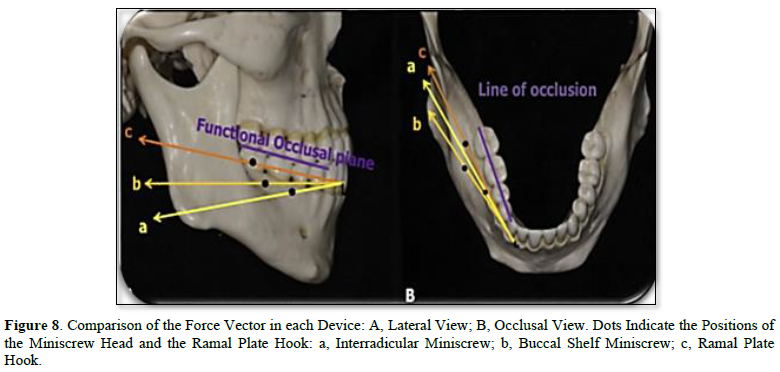
Tipping, anchorage loss, and flaring of the anterior teeth are common effects of non-compliant appliances, such as a distal extension lingual arch, Jones jig, or Franzulum appliance [8-10]. The use of transient skeletal anchorage devices has resolved these molar distalization problems (TSADs) [10,11]. Mini screws may need to be relocated during distalization if they are positioned between the interradicular spaces as this can interfere with the distalization procedure. This disadvantage was addressed by Poletti [12] placed a miniscrew in the retromolar region to distalize the lower dentition. However, it's possible that only one miniscrew on each side will not be strong enough to withstand the forces required for full arch distalization. Consequently, in two studies by Sugawara [13,14] a skeletal anchorage system was implanted at the mandibular body and the treatment's outcomes were evaluated.
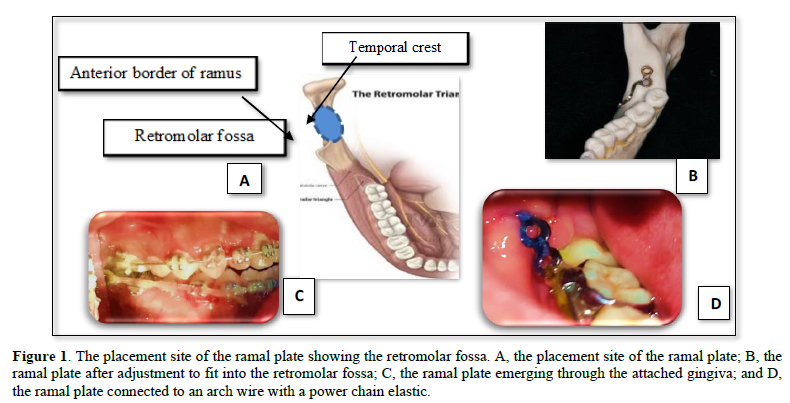
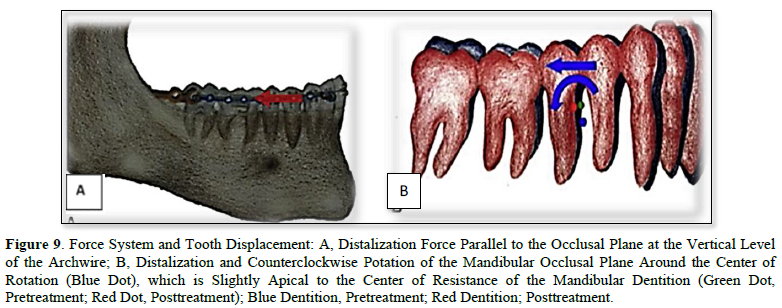
The distalization of the mandibular dentition has recently been reported as being facilitated by the use of a plate positioned at the ramus' retromolar fossa by Kook [15] Compared to buccal miniscrews, which are exposed through the movable vestibular mucosa and buccal cheek, this device, which is exposed through the retromolar region, may have a force vector that is more parallel to the occlusal plane and should be less abrasive. In Yemen, many studies indicated high rates of malocclusions with class I, where malocclusion class I being the most common followed by class II malocclusion, and class III malocclusion was also reported at significant rates [16-19]. The introduction of Ramal plate placement in the retromolar fossa as a new temporary skeletal anchorage device (TSAD) to remotely correct Class III skeletal malocclusions in Yemen could benefit oral health procedures that may correct and prevent the development of serious types of malocclusions thereafter in patients' lives. Thus, the purpose of this study was to introduce the placement of a ramal plate in the retromolar fossa as a new TSAD to correct class III skeletal malocclusion by distalization of mandibular dentition among Yemeni patients.
METHODS AND MATERIALS
A clinical cohort study was carried out. The sample consisted of pre-and post-treatment CBCT lateral cephalometric of 6 patients (3 males and 3 females; mean age 20±2 years) who received a ramal plate for mandibular molar distalization. In the Department of Orthodontic, Sana`a University, Al-Kuwait University Hospital. The sample size required to detect a difference of at least 1.5 units with a standard deviation of 2 units using a power of 0.8 and a probability of type I error (α) = 0.05 was 6 patients. Approval was obtained from the institution review master degree committee of Faculty of Dentistry, (20-01-222) and informed consent was obtained from all subjects. The inclusion criteria were:
- A patient over 18 years of age at the start of treatment
- Features of clinically validated and cephalometric Class III skeletal malocclusion, panoramic cone beam CT scan and with Class III dental malocclusion with more than half of the molar discrepancy
- Anterior cross bite
- A full set of permanent teeth with a low index of caries and periodontal disease
- Free from any systemic diseases or congenital anomalies
- They do not have previous orthodontic treatment
Appliance description: All patients were prepared to make miner operation at AL-Kuwait University Hospital under local anesthesia. The local anesthetic solution (2% lidocaine or Abniphrin with 1:80000 Adrenalin 1.8mL) was then administered as mandibular block for both sides, followed by orthodontic fixing treatment for alignment and arrangement teeth. A ramal plate is placed in the retromolar fossa, located between the anterior border of the mandibular ramus and the temporal crest Figure 1. After doing the flap in the retromolar area, the L-plate bending (Figure 2) (LeForte System; Jeil Medical, Seoul, Turkia; length of the short arm, 10 mm; length of the long arm, 20 mm; diameter, 2.5 mm) is adapted to fit the bone surface. The third molars are extracted during the procedure. The anterior hole of the plate that extends into the oral cavity is positioned horizontally to be 3 mm lateral to the buccal surface of the second molar, and between the buccal groove of the second molar and its distal surface, anterioposteriorly (Figure 1). The plates were fixed with 2 screws (Figure 3) with a pilot drill (Figure 4). Pilot holes were then created using a low-speed surgical hand piece at 800 rpm, under NaCl irrigation, 2 mm in diameter, and 6 mm in length by a bore drill. The flap (usually two flaps) is sutured above the plate, and the hook is extended beyond the mucosa, vertically to the level of the second molar tube and laterally within 3 to 6 mm horizontally to the buccal surface of the second molar. The power elastic chain may be looped around the front screw hole of the plate, or it may be snap-cut to convert to a hook to facilitate the placement of elastic straps or closed coil springs of nickel-titanium attached to 0.019-by-0.025-in arc-wire crimped hooks of stainless steel between the side cutouts and canines immediately after plate placement (Figure 1). Power elastics chain were attached from Ramal plate hooks to the hooks between the lateral and canine to deliver a force of 250 g to 400 g per side and were replaced every 3 weeks, during the insertion of the elastic chain, tension and pressure gauges were used in order to measure the force. Antibiotics and anti-inflammatory were prescribed after the operation as a cover-up. Painkillers were also prescribed for some time to relieve any pain after the surgery and during the stretch (Figure 5).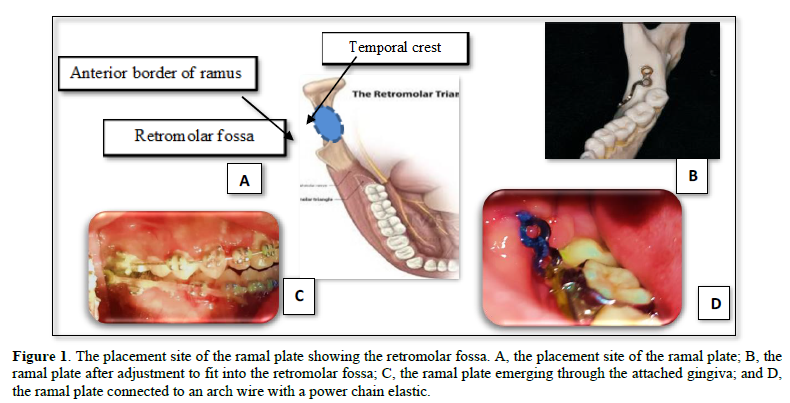
Important notice: There is a possibility that the posterior foramen may be close to the placement area when the ramal plate is inserted. However, the probability of this happening is between 9% and 25% [20-22]. Because the neurovascular bundle is connected to the pulp and periodontal tissues of the third molar through the foramen. Therefore, the placement position must be examined after flap reflection in relation to the position of this foramen.
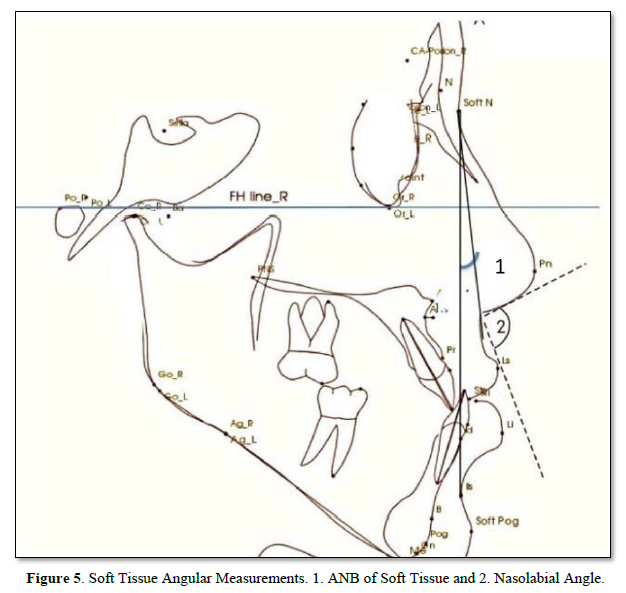
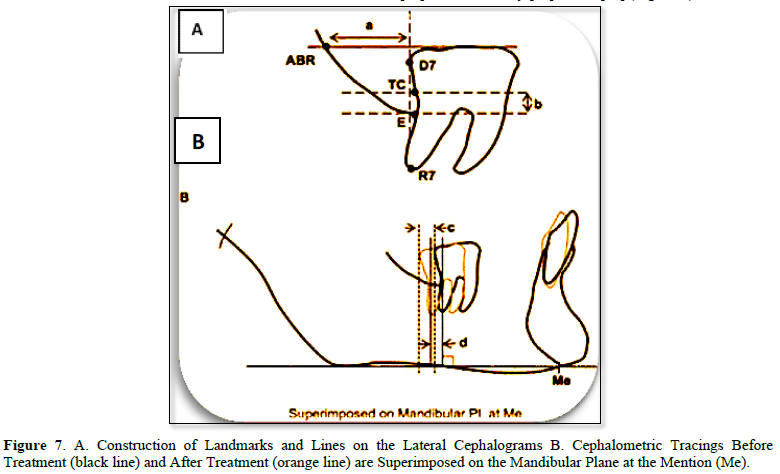
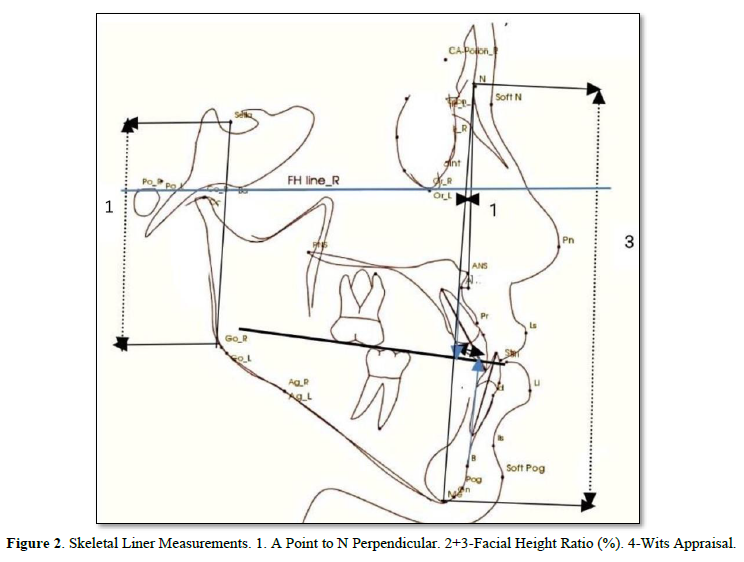
Cephalometric analysis: Pre and post treatment lateral cephalometric radiographs were digitized. All the subject heads were fixed by means of two ear rods inserted into the external auditory meati. The Frankfort horizontal plane was oriented parallel to the floor and the midsagittal plane was maintained parallel to and at a fixed distance of the film. A constant distance of (1745mm) was maintained between the x-ray source and midsagittal plane. The subject was asked to close the mouth in centric occlusion.
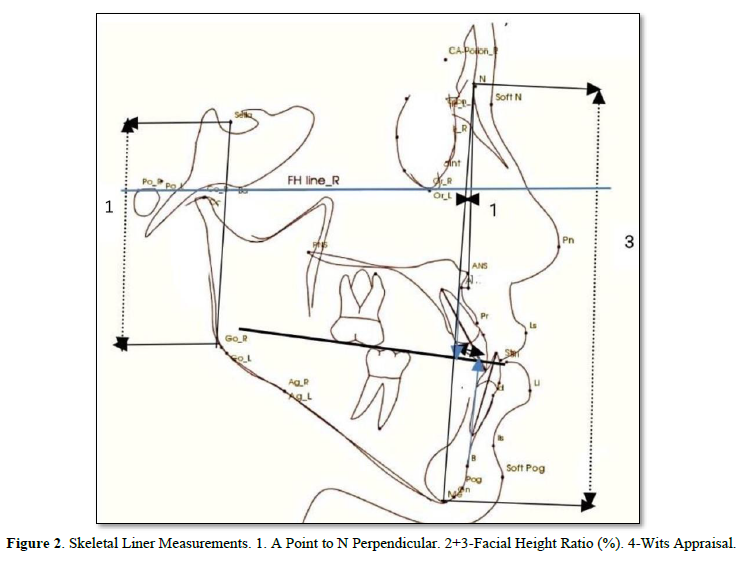
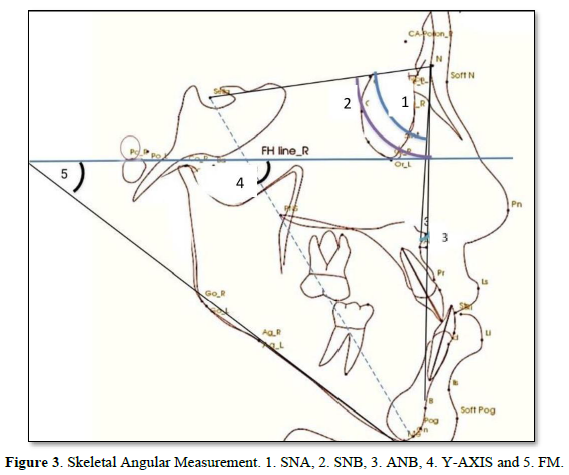
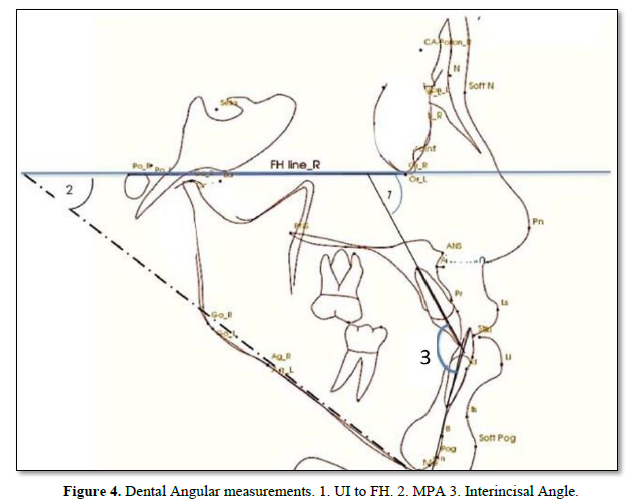
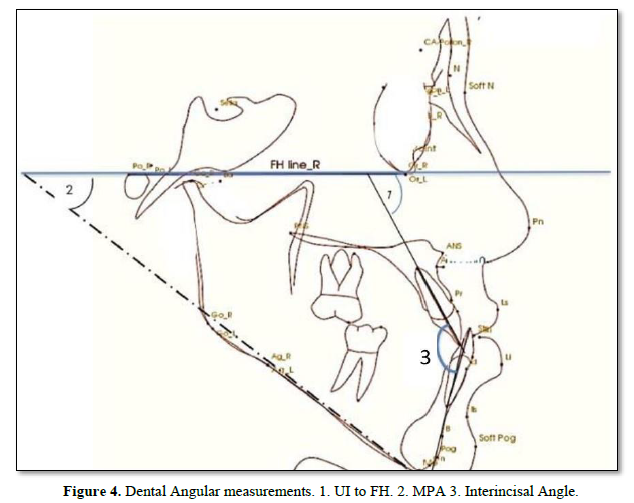
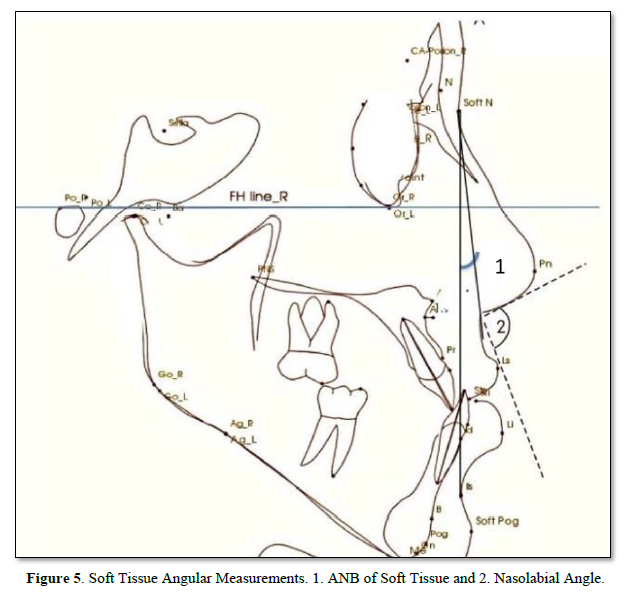
Eighteen linear and angular measurements were calculated electronically using the software In-Vivo-Dental-Intel Application Version 6.0 (Figures 2-5). The same examiner repeated the cephalometric digitization of three randomly selected cases two weeks later. To assess intra-examiner reliability, the intraclass correlation coefficient (ICC) was used. For all variables, the ICC ranged between 0.360 and 0.342.
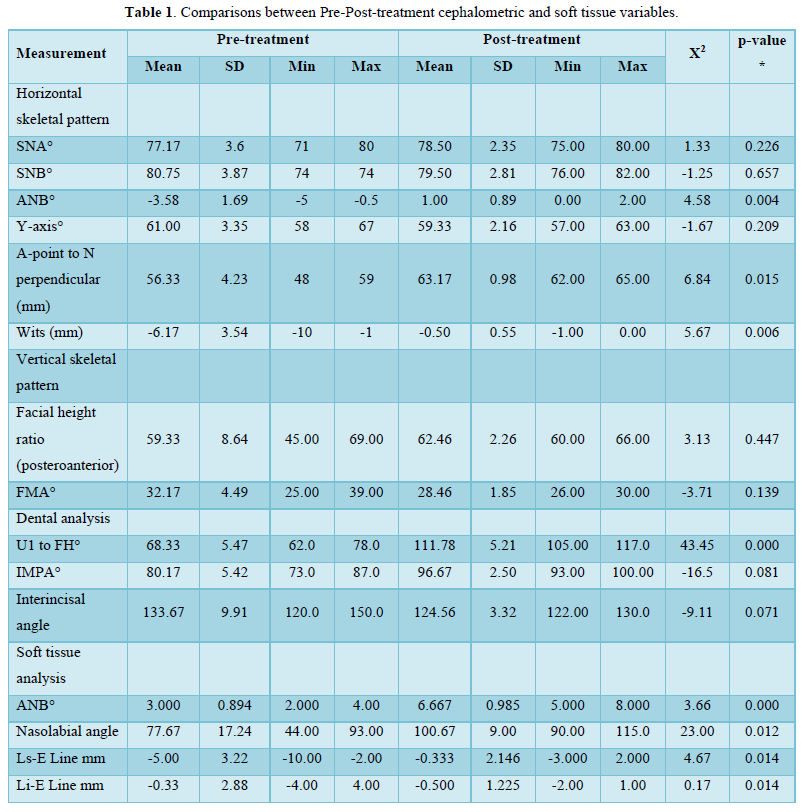
Statistical analysis: Some descriptive statistical analysis parameters were calculated using Minitab 20. All values presented were for measurements that were performed during the study, including horizontal and vertical skeletal patterns, dental analysis, and soft tissue analysis for patients in this study. The mean and the standard deviation (SD) for all measurements are presented for pre- and post-treatments. The minimum (Min) and maximum (Max) values for all measurements were also presented in Table 1. The differences between the means of the pre- and post-treatments were calculated by subtracting their means. The P-value was calculated using GLM ANOVA in Minitab 20 and compared to a p-value of ≤ 0.05 to find out if the treatments achieved the goal of this study.
RESULTS
In the evaluation of tooth movement in relation to the FH as craniofacial reference line, there was a significant in clinical observation and some of Cephalometric analysis. The total treatment time for distalization of a whole mandibular jaw was 7 months and 3weeks with a range of 7-8 months. But the total treatment as a finishing case took 36months.
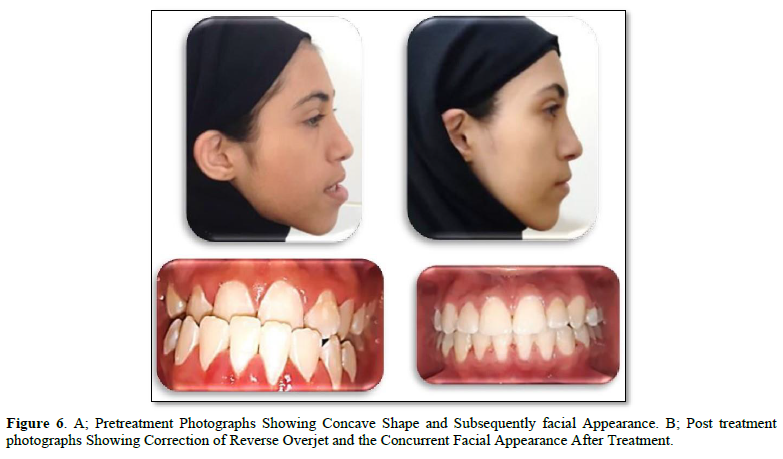
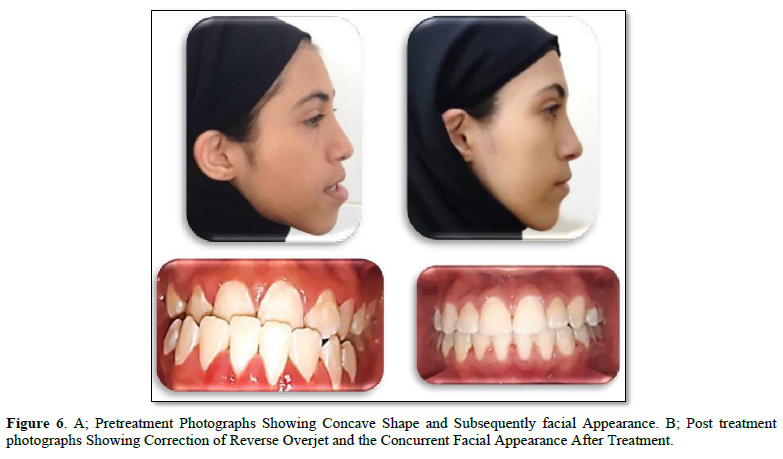
Clinical Observation: The following observations were seen in all cases as in Figure 6:
- The normal overjet of an anterior teeth and canine (2±2mm of overjet), molar Class I relationship (5±2mm distalized) was seen in all patient in the end of 7-8 months since the distalization procedure started.
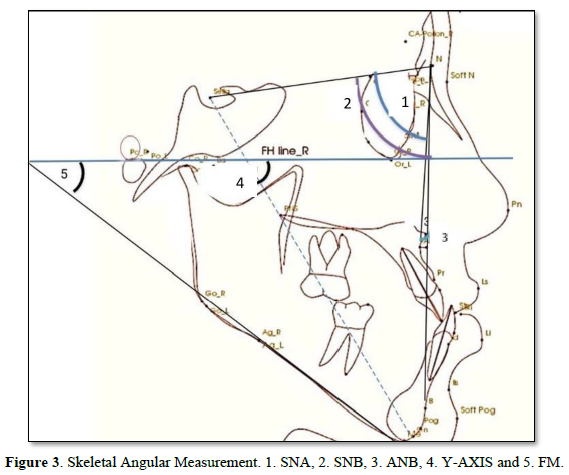
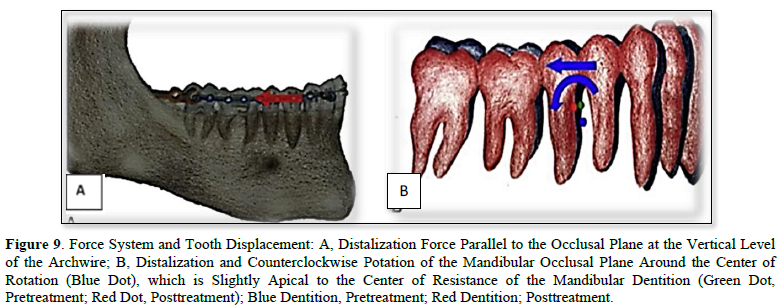
- By applying a force (250-400g) parallel to the functional occlusal plane and Counterclockwise around a point just apical to the mandibular dentition's center of resistance, the mandibular occlusal plane was moved distalized and no rotated.
- As seen in the patients, this resulted in distalization of the entire dentition, as well as posterior tooth intrusion and front tooth extrusion.
- Additionally, in all patients, there were no signs or symptoms of gingival recession, mobility, or bone loss.
The Result Cephalometric Analysis will be Presented as a follow: Angle degree measurements were taken before and after treatments for SNA°, SNB°, ANB°, and Y-axis°. Statistical analysis showed in Table 1 that there is a significant p-value ≤ 0.05 between some of the measures that are important and considered critical to evaluating the treatments. In the evaluation of skeletal variables, there was a significant change in the sagittal relationship between the mandible and maxilla (Wits, 2.4 mm; p =0.006), A point-nasion-B point (ANB; p =0.004) and A-point to N perpendicular (mm). However, the sella-nasion-A point (SNA) angles, and the sella-nasion-B point (SNB) were not changed significantly. Moreover, the FMA angle did not increase significantly and facial height ratio (Table 1). In the evaluation of dental variables, there was a significant change in (U1 to FH°, p=0.000, IMPA, p=0.018, and interincisor Angle, p=0.017). In the evaluation of soft tissue, there was significant effect on upper lip position (nasolabial angle, p = 0.000; Esthetic line-upper lip, p = 0.014). However, the lower lip showed a significant retraction of 3.2 mm (p = 0.014).
Values are presented as mean ± standard deviation.
ANB, A point-nasion-B point; SNB, sella-nasion-B point; Pog, pogonion; SNA, Wit’s appraisal, Y-axis N, nasion
DISCUSSION
The diagnosis and treatment of Class III malocclusion are considered to be one of the most difficult problems for orthodontists because its etiology is complicated. Not much literature has been published about treatment of Class III malocclusion with fixed appliances using recent application of a Novel ramal plate (TSADs) conducted in Yemen, and previous research has been conducted on dental caries, oral and facial abscesses of odontogenic origin, localized aggressive gingivitis (LAP), periodontitis, bacterial and fungal oral infections, interleukin-1 levels in human gingival sulcus, prevalence and association of the maxillary sinus septum with sex and location in the maxillary among adults, factor analysis and pattern of permanent tooth extraction, effect of removable dentures on aerobic bacterial colonization, and clinical effects of platelet-rich fibrin (prf) after surgical extraction of impacted lower third molars [23-33], there is no information regarding the treatment of class III malocclusion in Yemeni adult. Therefore, it was the aim of this work to study treatment of class III malocclusion in Yemeni adult.
In this study, the treatment time for distalization treatment ranged from 7 to 8 months, including correction of the negative overjet of an anterior tooth as well as the canine and molar Class I relationship, which were seen in all patients at the end of 7-8 months from the initiation of this medically exclusion procedure and photos. The recent application of TSADs to split the dental arch of the mandible reduced the range of orthodontic treatment in our study and this is similar to the findings of previous studies and confirmed the previous results [16,34-38].
Clinical resulting from the treatment: In the current study, all of the cases had correction of negative overjet and class I canine and molar relationship (Figure 6), these results agreed with Yu [34] Yeon [35] Kook [38]. Some patients included in our study had discrepancies greater than ½ or 2/3 molar relation Class III, this differs from other research, as their research included patients with discrepancies of ½ or 2/3 molar relation of Class III molar relationship, and this may have resulted in a reduction of the mean dimension in our study, as confirmed by some other studies also Ludwig [39]. Therefore, we show the full capacity of the ramal plate where some patients had a severe condition unlike the rest of the research by Yu [34], Kook [38].
Although the miniscrew can only pull the mass of teeth to a certain extent, because of the inter-radicular space, it is difficult to distalize more than 2-3 mm with the miniscrew because the interradicular space [38,39] but with ramal plates as in the current study it distilize more than 4± 2.5mm and this is similar to that reported by Kim [40]. Also, plates, in general, can withstand high forces, and their stability is enhanced by the use of two screws [6,38]. Several studies have found that miniplates fail at a lower rate than miniscrews [38] The plate's hook exposed through the retromolar area, which may cause less discomfort than when it is exposed through the moveable vestibular mucosa, and contrary to the report of excessive distal tipping with mini screw, the distalization with distal tipping ratio was minimum with ramal plate as in the current study and recent conducted studies [15,37].
Clinically the standard overjet of an anterior teeth and canine, molar Class I relationship was seen in the all patient by used the ramal plate for distalization procedure started the current study clinical result agreed with that of [34,35,38]. All our patients received orthodontic treatment by applying a force parallel to the functional occlusal plane and counterclockwise around a point just apical to the mandibular dentition's center of resistance using an elastic bower chain. The mandibular occlusal plane was moved distalization and not rotated, this result is in accordance with the results of [34,35,39,40] (Figures 7-9). As seen in our patients clinically, this resulted in distalization of the entire dentition, as well as posterior tooth intrusion and front tooth extrusion. This result agreed with that reported [34,35,38]. Additionally, in all patients of the current study, there were no signs or symptoms of gingival recession, mobility, or bone loss. This result is in comparison, with studies by Yu [34], Krishnamurthy [36], Kook [38] (Figure 6).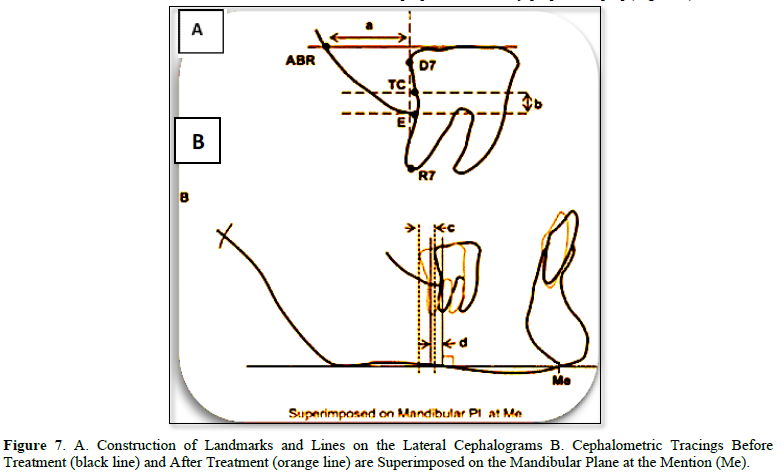
Lateral CBCT Cephalometric: Selected CBCT lateral cephalometric variables were identified for each cephalogram, representing skeletal, dentoalveolar, and soft tissue measurements (Figures 2-5).
Skeletal Change: Analysis of the treatment result indicated that there was a statistically significant change in the sagittal relationship between the mandible and maxilla. This result was highly statistically significant Wit’s appraisal, p = 0.006. This result agreed with Yu [34], Yeon [35] Also, the current study result got a high statistically significant ANB° P-Value = 0.004 as shown in Table 1, this result was not in agreement with [34] However, statistically significant levels of SNA° and SNB° did not change significantly between pre- and post-treatment (Tables 1).
The two variable of Facial high ratio and FMA° result indicated limited craniofacial change after treatment since no statistically significant difference observed in most of cephalometric Skeletal angular parameter (Table 1). This result is agreed with that of Yu [34] but was disagreed with that reported by Yeon [35] where the FMA° had significant result.
Dental Changes: Evaluation of the post-treatment outcome showed improvement in most of the bilateral alveolar variables as shown in Table 1 by highly significant in U1 to FH °P-Value = 0.000, IMPA °p-Value = 0.081 as well as the interincisal angle. [38] did not perform any statistical analysis in their research on this variable, and [34] did not take the same measurement parameter in their statistical analysis as the one that worked in this research. Our findings indicate that correction of the anterior reverse overjet and overlay without significant change in the mandibular plane resulted in distalization of the mandibular teeth. This study improvement of interincisor angle was very significant while U1 to FH° and IMPA° were statistically highly significant as shown in Table 1.
Soft Tissue Changes: In the current study, four variables were used in an attempt to understand possible changes in different aspects of face, such as ANB° of soft tissue, nasolabial angle, upper lip and lower lip of esthetic plane line. Evaluation of the soft tissue profile in the 6 patients revealed an improvement a high statistically significant, especially in the ANB° of soft tissue has a high statistically significant p-value =0.000 as shown in Table 1. There is no agreement between our study and Yu [34] where there was no statistically significant effect on the position of the upper lip and nasolabial angle but their results agreed with our study in the lower lip.
CONCLUSION
After alignment and leveling the patients using recent application of Noval ramal plate in retromolar fossa, the retromolar fossa is an anatomically appropriate location. The force vectors that result is parallel to the occlusal plane, resulting in efficient molar distalization. With ramal plates, there was no significant change in the vertical position of the mandibular molar or in the MP angle. In the evaluation of dental variable, there were a statically significant in U1 to FH°, IMPA° and Interincisor Angle. In the evaluation of soft tissue there was a statically significant in Nasolabial Angle, Ls-E Line (mm), and Li-E line (mm). Therefore, ramal plates are an effective treatment option for Class III patients who are apprehensive about undergoing extraction teeth and or orthognathic surgery for mandibular complete arch distalization.
ACKNOWLEDGMENTS
The authors thank the Faculty of Dentistry, Sana'a University, Sana'a, and Yemen for their generous support.
CONFLICT OF INTEREST
No conflict of interest associated with this work.
- Jokić D, Jokić D, Uglešić V, Macan D, Knežević P (2013) Soft tissue changes after mandibular setback and bimaxillary surgery in Class III patients. Angle Orthod 83(5): 817-823.
- Janson G, de Souza JE, Alves Fde A, Andrade P Jr, Nakamura A, et al. (2005) Extreme dentoalveolar compensation in the treatment of Class III malocclusion. Am J Orthod Dentofacial 128(6): 787-794.
- Neto JV (2014) Compensatory orthodontic treatment of skeletal Class III malocclusion with anterior crossbite. Dental Press J Orthod 19(1): 113-122.
- Hu H, Chen J, Guo J, Li F, Liu Z, et al. (2012) Distalization of the mandibular dentition of an adult with a skeletal Class III malocclusion. Am J Orthod Dentofacial Orthod 142(6): 854-862.
- Saito I, Yamaki M, Hanada K (2005) Nonsurgical treatment of adult open bite using edgewise appliance combined with high-pull headgear and class III elastics. Angle Orthod 75(2): 277-283.
- Chen CH, Hsieh CH, Tseng YC, Huang IY, Shen YS, et al. (2007) The use of miniplate osteosynthesis for skeletal anchorage. Plast Reconstr Surg 120(1): 232-235.
- Sugawara J, Daimaruya T, Umemori M, Nagasaka H, Takahashi I, et al. (2004) Distal movement of mandibular molars in adult patients with the skeletal anchorage system. Am J Orthod Dentofacial Orthop 125(2): 130-138.
- Kinzinger G, Gross U, Diedrich P (2000) Fixed lingual arch appliance for compliance-free unilateral molar distalization in the mandible. Three case studies. J Orofac Orthop 61(6): 440-450.
- O'Donnell S, Nanda RS, Ghosh J (1998) Perioral forces and dental changes resulting from mandibular lip bumper treatment. Am J Orthod Dentofacial Orthop 113(3): 247-255.
- Muse DS, Fillman MJ, Emmerson WJ, Mitchell RD (1993) Molar and incisor changes with Wilson rapid molar distalization. Am J Orthod Dentofacial Orthop 104(6): 556-565.
- Jing Y, Han X, Guo Y, Li J, Bai D (2013) Nonsurgical correction of a Class III malocclusion in an adult by miniscrew-assisted mandibular dentition distalization. Am J Orthod Dentofacial Orthop 143(6): 877-887.
- Poletti L, Silvera AA, Ghislanzoni LT (2013) Dentoalveolar class III treatment using retromolar miniscrew anchorage. Prog Orthod 14: 7.
- Sugawara J, Kanzaki R, Takahashi I, Nagasaka H, Nanda R (2006) Distal movement of maxillary molars in nongrowing patients with the skeletal anchorage system. Am J Orthod Dentofacial Orthop 129(6): 723-733.
- Sugawara Y, Kuroda S, Tamamura N, Takano-Yamamoto T (2008) Adult patient with mandibular protrusion and unstable occlusion treated with titanium screw anchorage. Am J Orthod Dentofacial Orthop 133(1): 102-111.
- Kook YA, Park JH, Bayome M, Kim S, Han E, et al. (2016) Distalization of the mandibular dentition with a ramal plate for skeletal Class III malocclusion correction. Am J Orthod Dentofacial Orthop 150(2): 364-377.
- AL-Awadi TAM, AL-Haddad KA, Al-labani MA, Al-Shamahy HA, Shaga-aldeen HM (2020) Prevalence of malocclusion among Yemeni children of primary schools. Uni J Pharm Res 5(1): 1-6.
- Yehia LAB, AL-Haddad KA, Al-labani MA, Al-Shamahy HA, Shaga-aldeen HM (2020) Occlusal characteristics of the primary dentition among a sample of Yemeni pre-school children. Uni J Pharm Res 5(1): 7-12.
- Bamashmoos KAO, Alhasani AH, Al-Akwa AAY, Zabara AQMQ (2020) Prevalence of premature loss of primary teeth at the age of 6-10 years in Sana’a city, Yemen. Uni J Pharm Res 5(4): 1-6.
- Zabara AQMQ, Al-Kholani AIM, Al-Shamahy HA, Al-Kibsi TAM, Al-Akwa AAY, et al. (2022) Resolution of factors and pattern of permanent dental extraction in selected dental clinics in Sana’a city, Yemen. Uni J Pharm Res 7(4): 1-8.
- Bilecenoglu B, Tuncer N (2006) Clinical and anatomical study of retromolar foramen and canal. J Oral Maxillofac Surg 64(10): 1493-1497.
- Rossi AC, Freire AR, Prado GB, Prado FB, Botacin PR et al, (2012) Incidence of retromolar foramen in human mandibles: Ethnic and clinical aspects. Int J Morphol 30: 1074-1078.
- von Arx T, Hänni A, Sendi P, Buser D, Bornstein MM (2011) Radiographic study of the mandibular retromolar canal: An anatomic structure with clinical importance. J Endod 37(12): 1630-1635.
- Alhadi YAA, Al-Shamahi NY, Al-Shamahy HA, Al-Najhi AMM, Al-Shamahy HA, et al. (2022) Maxillary sinus septa: Prevalence and association with gender and location in the maxilla among adults in Sana’a city, Yemen. Uni J Pharm Res 7(3): 1-6.
- Alhadi YAA, Al-Kibsi TAM, Al-Shamahy HA, Aldeen YAAS (2022) Surgical site infections: prevalence, associated factors and antimicrobial susceptibility patterns of the bacterial isolates among postoperative patients in Sana’a, Yemen. Uni J Pharm Res 7(3): 1-6.
- Abbas AM, Al-Kibsi TAM, Al-Shamahy HA (2020) Characterization and antibiotic sensitivity of bacteria in orofacial abscesses of odontogenic origin. Uni J Pharm Res 5(6): 36-42.
- Al-Akwa AA, Zabara A, Al-Shamahy HA (2020) Prevalence of Staphylococcus aureus in dental infections and the occurrence of MRSA in isolates. Uni J Pharm Res 5(2): 1-6.
- Al-Deen SSH, Al-Ankoshy AAM, Al-Shamahy HA, Al-Kibsi TAM, AL-Haddad KA, et al. (2021) Porphyromonas gingivalis: Biofilm formation, antimicrobial susceptibility of isolates from cases of Localized Aggressive Periodontitis (LAP). Uni J Pharm Res 6 (4): 1-6.
- AL-Haddad KA, Al-Najhi AMM, Al-Akwa AAY (2007) Antimicrobial susceptibility of Aggregatibacter actinomycetemcomitans isolated from Localized Aggressive Periodontitis (LAP) Cases. J Dent Oral Health Adv Res 103: 1-6.
- Alhasani AH, Ishag RA, Al Shamahy HA, Abdullah A, Shamahy AL, et al. (2020) Association between the Streptococcus mutans biofilm formation and dental caries experience and antibiotics resistance in adult females. Uni J Pharm Res 5(6): 1-3.
- Al-Shamahy HA, Abbas AMA, Mohammed MAM, Alsameai AM (2018) Bacterial and fungal oral infections among patients attending dental clinics in Sana’a City-Yemen. Onl J Dent Oral Health 1(1): 1-6.
- Al-dossary OAI, Al-Kholani AIM, Al-Shamahy HA (2022) Interleukin-1β levels in the human gingival sulcus: Rates and factors affecting its levels in healthy subjects. Uni J Pharm Res 7(5): 25-30.
- Al-Haddad K, Al-Najhi MM, Al-Kholani AIM, Al-Shamahy HA, Alrubaidi YA, et al. (2023) Effect of removable dentures on colonization of aerobic bacteria in the oral cavity and antibiotic pattern of the common isolated bacteria. Uni J Pharm Res 7(6): 1-8.
- Makki KIF, Abbas AMA, Alhadi YAA, Al-Shamahy HA (2023) Clinical effects of Platelets Rich Fibrin (PRF) following surgical extraction of impacted lower third molars among a sample of Yemeni adults. Uni J Pharm Res 7(6): 8-14.
- Yu J, Park JH, Bayome M, Kim S, Kook YA, et al. (2016) Treatment effects of mandibular total arch distalization using a ramal plate. Korean J Orthod 46(4): 212-219.
- Yeon BM, Lee NK, Park JH, Kim JM, Kim SH, et al. (2022) Comparison of treatment effects after total mandibular arch distalization with miniscrews vs ramal plates in patients with Class III malocclusion. Am J Orthod Dentofacial Orthop 161(4): 529-536.
- Krishnamurthy S, Prashantha GS, Sagarkar R, Bhaduri N, Padmanathan R, et al. (2022) En-masse distalization of mandibular dentition with ramal miniplate for correction of Class III malocclusion: A Case Report. J Clin Diagnostic Res 16(10): ZD08-ZD11.
- Chang C, Liu SS, Roberts WE (2015) Primary failure rate for 1680 extra-alveolar mandibular buccal shelf mini-screws placed in movable mucosa or attached gingiva. Angle Orthod 85(6): 905-910.
- Kook Y-A, Park JH, Bayome M, Kim S, Han S, et al. (2016) Distalization of the mandibular dentition with a ramal plate for skeletal Class III malocclusion correction. Am J Orthod Dentofacial Orthop 150: 364-377.
- Ludwig B, Glals B, Kinzinger GSM, Liettz T, Lisson JA (2011) Anatomical guidelines for miniscrew insertion: vestibular interradicular sites. J Clin Orthod 45: 165-173.
- Kim YH, Han UK, Lim DD, Serraon ML (2000) Stability of anterior open bite correction with multiloop edgewise archwire therapy: A cephalometric follow-up study. Am J Orthod Dentofacial Orthop 118: 43-54.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Advance Research on Alzheimers and Parkinsons Disease
- Journal of Rheumatology Research (ISSN:2641-6999)